By Jackie Scrivanich, Contributing Writer
When I got pregnant with my first child, I found myself researching so many new things. I would spend hours reading books, talking to women I trusted, and scouring the internet. I got lost in all of the different pregnancy complications and if I am honest, it made me worry a bit. So many things could go wrong. Knowing what complications are truly cause for concern, however, can be helpful in planning a natural birth, and knowing when deviating from one’s natural birth plan truly is warranted.
One of the things that I wanted dearly was a homebirth. While I was reading about all of the different pregnancy complications, placenta previa was mentioned. So I went searching for what it was, and how people get it, and what can be done about it. I found out a lot of information, and it was not all that comforting. Homebirth would pretty much be out of the picture if I had placenta previa. That thought in itself was upsetting. Then I read that women with this complication will most likely need a cesarean!
I went to my 20 week ultrasound and although my placenta was anterior and slightly low, it was not low enough to cover my cervix. While I did not have to deal with having placenta previa, many women do.
What is Placenta Previa?
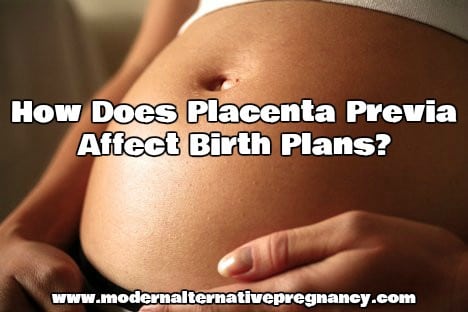
Placenta Previa is an overlap of the placenta over the cervix. Normally as a woman’s uterus grows, the placenta moves up towards the top of the womb. For one in 200 women, however, their placentas stay low and cover, or partially cover, their cervix (Source).
There are four grades of placenta previa, going from minor to major:
Grade 1 – (minor) the placenta is mainly in the upper part of the womb, but some extends to the lower part.
Grade 2 – (marginal) the placenta reaches the cervix, but doesn’t cover it.
Grade 3 – (major) the placenta partially covers the cervix.
Grade 4 – (major) the placenta completely covers the cervix (most serious type of placenta previa). (Source)
The following picture shows exactly what normal placental placement looks like versus what placenta previa looks like:
What Causes Placenta Previa?
There are theories for what causes placenta previa, but there is no clear answer. Some think it is due to late implantation, while others hypothesize that it could be due to uterine scarring from things like a previous cesarean.
That is the frustrating part of placenta previa, the fact that it just happens and there is not much you can do about it. And being diagnosed with it can change your entire birth plan.
How Do I know if I Have Placenta Previa?
Placenta previa is normally easy to diagnose. Most women are diagnosed at their 20 week ultrasound if they choose to get one. There is a reported incidence of 1-15% through the use of the second trimester ultrasound (Source). When a pregnant woman goes in for an ultrasound, the doctor is looking for a certain measurement of the placenta from the cervix. If there is an indication of the placental edge reaching or overlapping the cervix, “a follow-up examination for placental location in the third trimester is recommended” (Source). While the placenta can and does move during pregnancy, an overlap “of more than 15 mm is associated with an increased likelihood of placenta previa at term” (Source).
Other women may choose not to get an ultrasound, due to various reasons. If these women have placenta previa it usually presents itself with “painless third trimester bleeding” (Source). In a small number of women bleeding does not happen until they are in labor.
What Can I Do About Placenta Previa?
Not to be the bearer of bad news, but there is not much that can be done about placenta previa. You either have it or you do not. And if you do it will either clear up on its own or it will not.
It is very important to note, however, that many women who go in for their second trimester ultrasound and get diagnosed with placenta previa or partial placenta previa, or even just a low lying placenta, will not have an issue later in pregnancy. There is a “high-resolution rate for placenta previas diagnosed early in pregnancy” (Source). Chances are high of resolution if you are diagnosed with marginal placenta previa; “greater than 98% of marginal placenta previas resolved, with complete resolution of those diagnosed in the second trimester” (Source).
Being aware of the position of your placenta is very important. Not only does it affect where and how you can birth, placenta previa, in rare cases, can be dangerous. Some women might not even bleed at all during their pregnancies, but “placenta previa can be potentially life threatening, as it is possible to lose your entire blood volume in 10 minutes” (Source).
Can I Have a Vaginal Birth if I Have Placenta Previa?
For those that get to the end of pregnancy and still have a placenta previa diagnosis, your birth will be affected by this. Your baby cannot pass through your cervix and vaginal canal if your placenta is covering or even partially covering your cervix.
When a doctor looks at your ultrasound, and there is an overlap “of 20 mm or more at any time in the third trimester [it] is highly predictive of the need for Caesarean section” (Source). Any degree of overlap after 35 weeks is an indication that cesarean is the only option for delivery” (Source).
While cesarean is the recommendation for women with placenta previa, “women with a low-lying placenta have at least 60% chance of a vaginal birth, but should be monitored for post-partum hemorrhage” (Source). So there is hope for those with low-lying placentas.
How Does This Affect Birth Plans?
For most women, the plan for birth is not cesarean. So placenta previa will affect the birth plans for many women, especially for those like me who were planning a homebirth.
While rare, placenta previa can affect any of us during any pregnancy. It is concerning just because of that. It has no cause, and the other solution is to wait and see if it resolves itself. So through time, and possibly bed rest, you can possibly see the issue resolve itself. If it does then you can follow your original birth plan.





I have a friend who is currently planning a c section due to her second placenta pervia. She has recently discovered that it might be possible to still provide her baby with natural bacteria from the vagina. She is wanting to know more information on this, so I was wondering if you had any to share?
Much appreciated, April